Late effects of radiotherapy treatment
Help, support and information for the long-term side effects of radiotherapy.
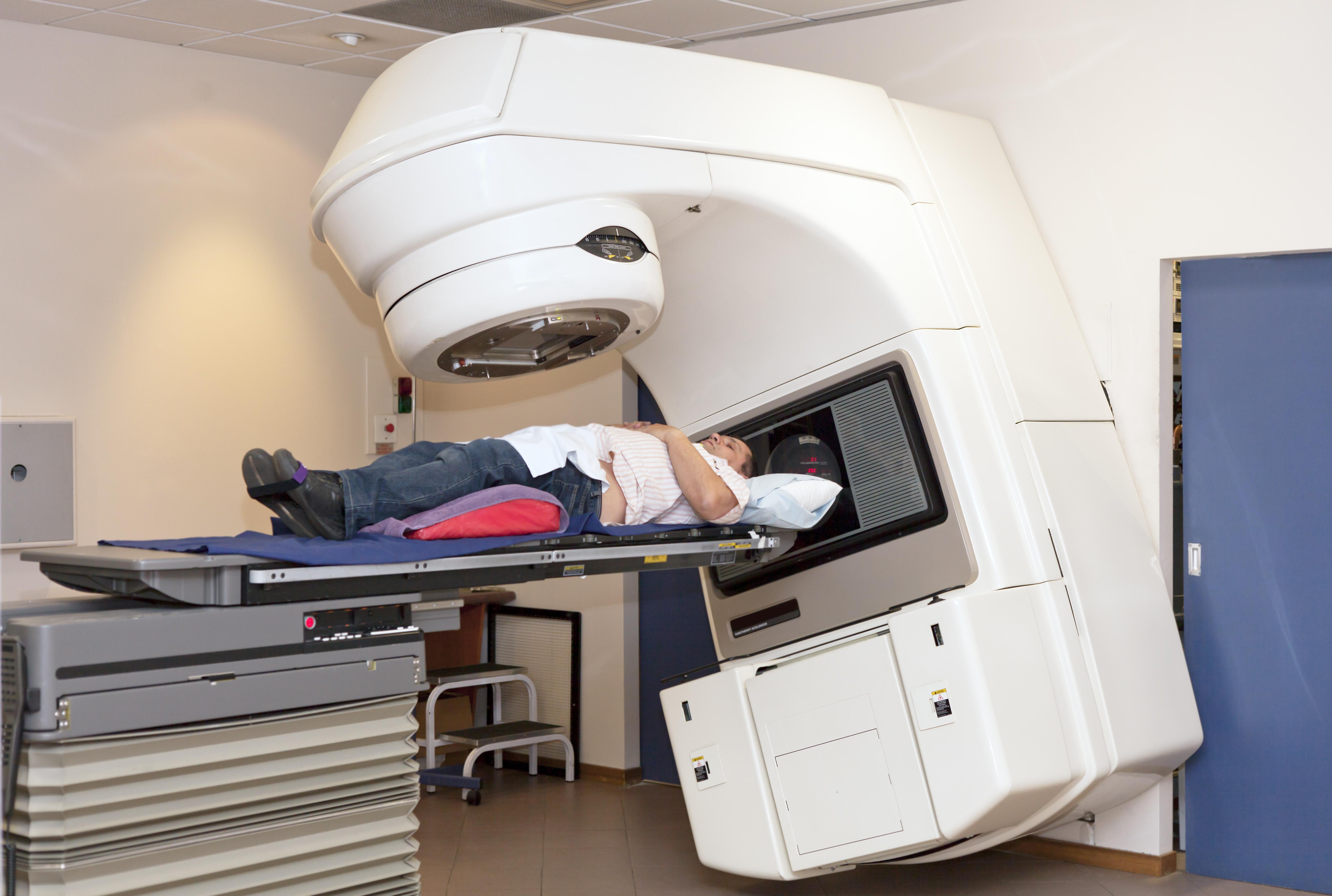
Pelvic Radiation Disease (PRD) is defined as one or more ongoing (chronic) symptoms
of variable complexity that may affect people who have previously had radiotherapy to
the pelvic region to treat their cancer. Pelvic Radiation Disease Association.
The Pelvic Radiation Disease Association (PRDA) is a patient charity dedicated to improving the care of patients with PRD. The website provides useful information for patients suffering with symptoms. This includes practical help and an online community.
Adapted from the The Royal College of Radiologists (RCR) prostate cancer consent form.
The Royal College of Radiologists have put together disease- and site-specific national consent forms. These are intended to support healthcare professionals. They make sure that patients have advice about the benefits and side effects of treatment that is:
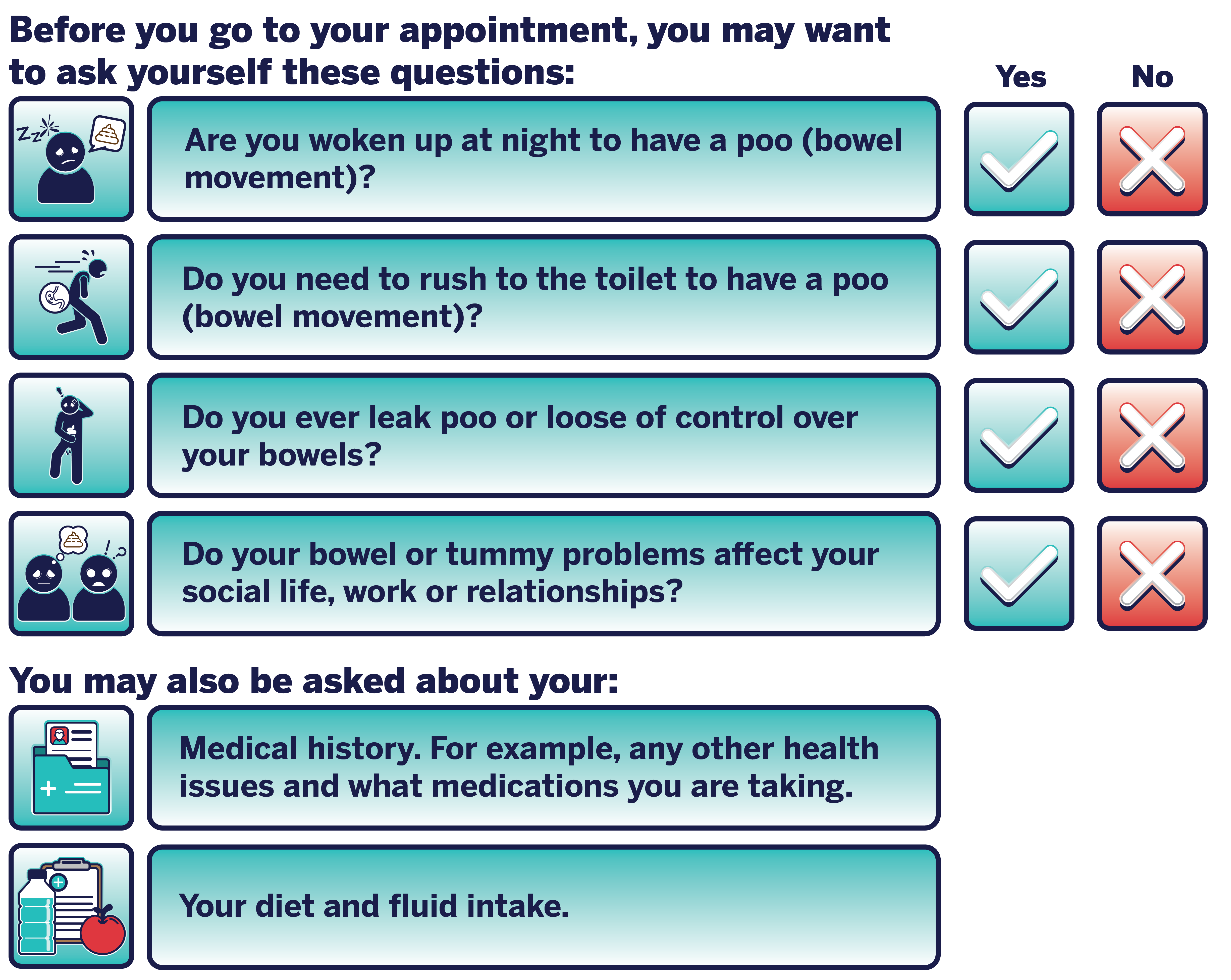
The first step will be to talk to your GP or healthcare team. They will ask you questions about your symptoms. For example:

They may then:
The team will ask you:

They are often run by specialist therapeutic radiographers.
They also have access to a wider team of specialist dieticians and continence specialists.
What do they do?
They aim to help people to live well with the late effects of radiotherapy.
They can offer:


Visit our page on getting support for sexual problems, for more information. This link will open in a new tab.
This will depend on what symptoms you are experiencing. See below for more information on the tests you may have for each symptom.
In some cases, you may have to have a camera passed into your bottom. This can be:

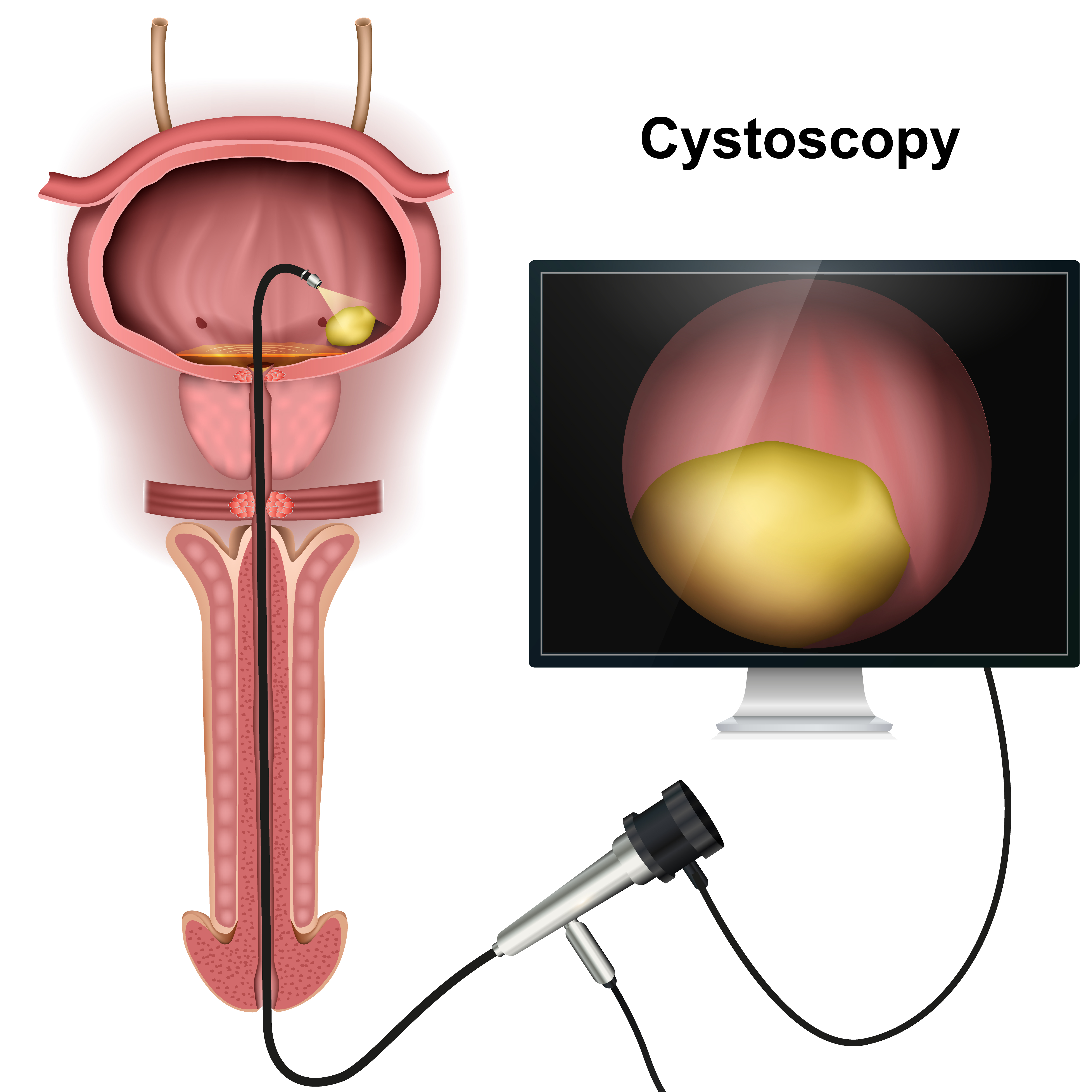
However, if they are worried, your GP may refer you the urology team. They will carry out more tests. This may be a cystoscopy.
In a cystoscopy a camera is passed into your bladder. This is done under a local anaesthetic. It can be done under a general anaesthetic if you are concerned about being awake during the procedure. More information can be found on the NHS website. This link will open in a new tab.

Problems with peeing may include:
In addition:
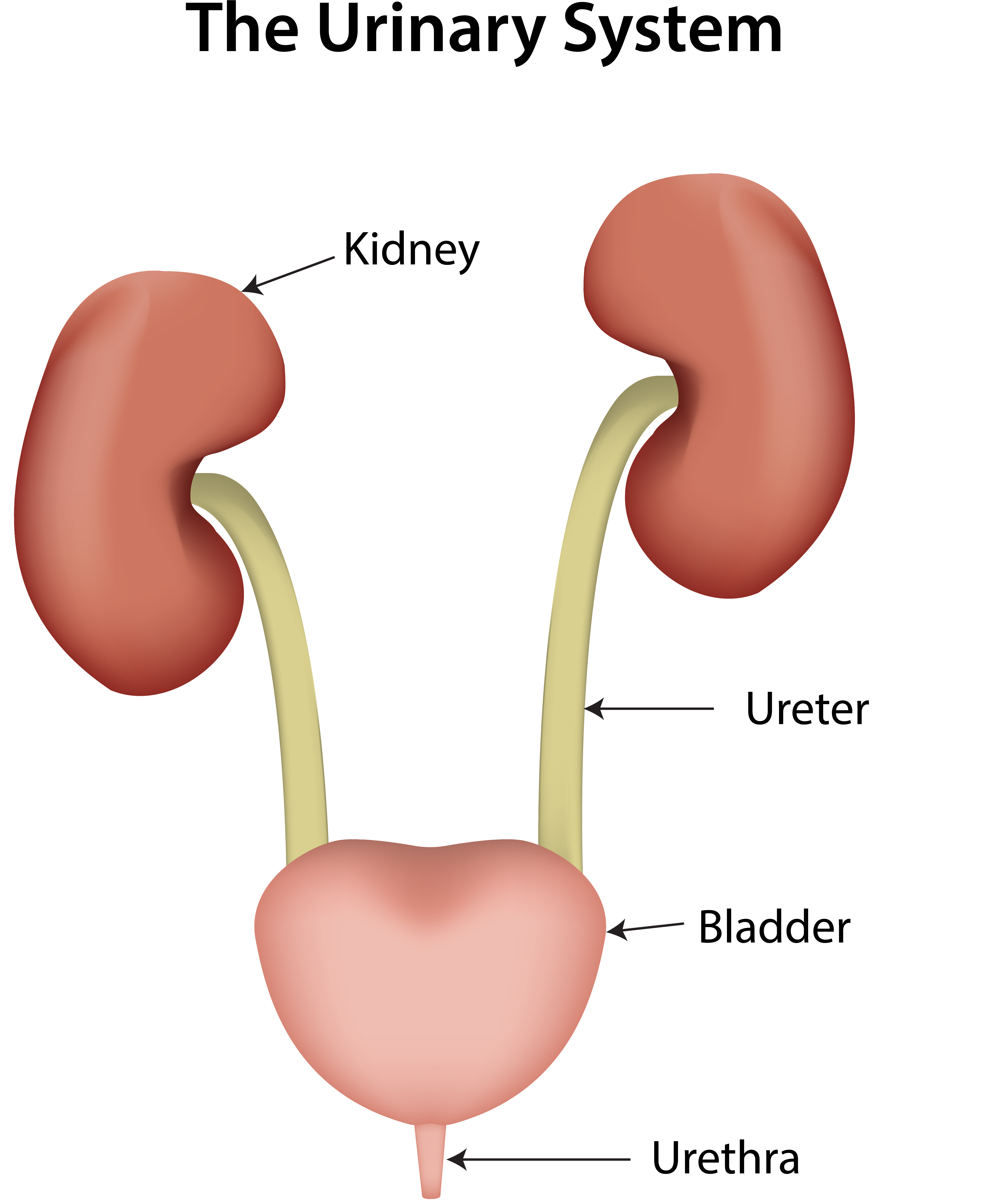
If you have any of these symptoms it may mean that you have narrowing or scarring in the tube that goes from your bladder to the outside (urethra). This is called urethral stricture.
Your GP may talk to you about medicines that can help to reduce the leaking. If these do not work, they may refer you to a urologist who will carry out further tests. These tests may include:
A CT urogram.
You may also be asked to keep a bladder diary. Take a look at these examples. Both of these links will open in a new tab:
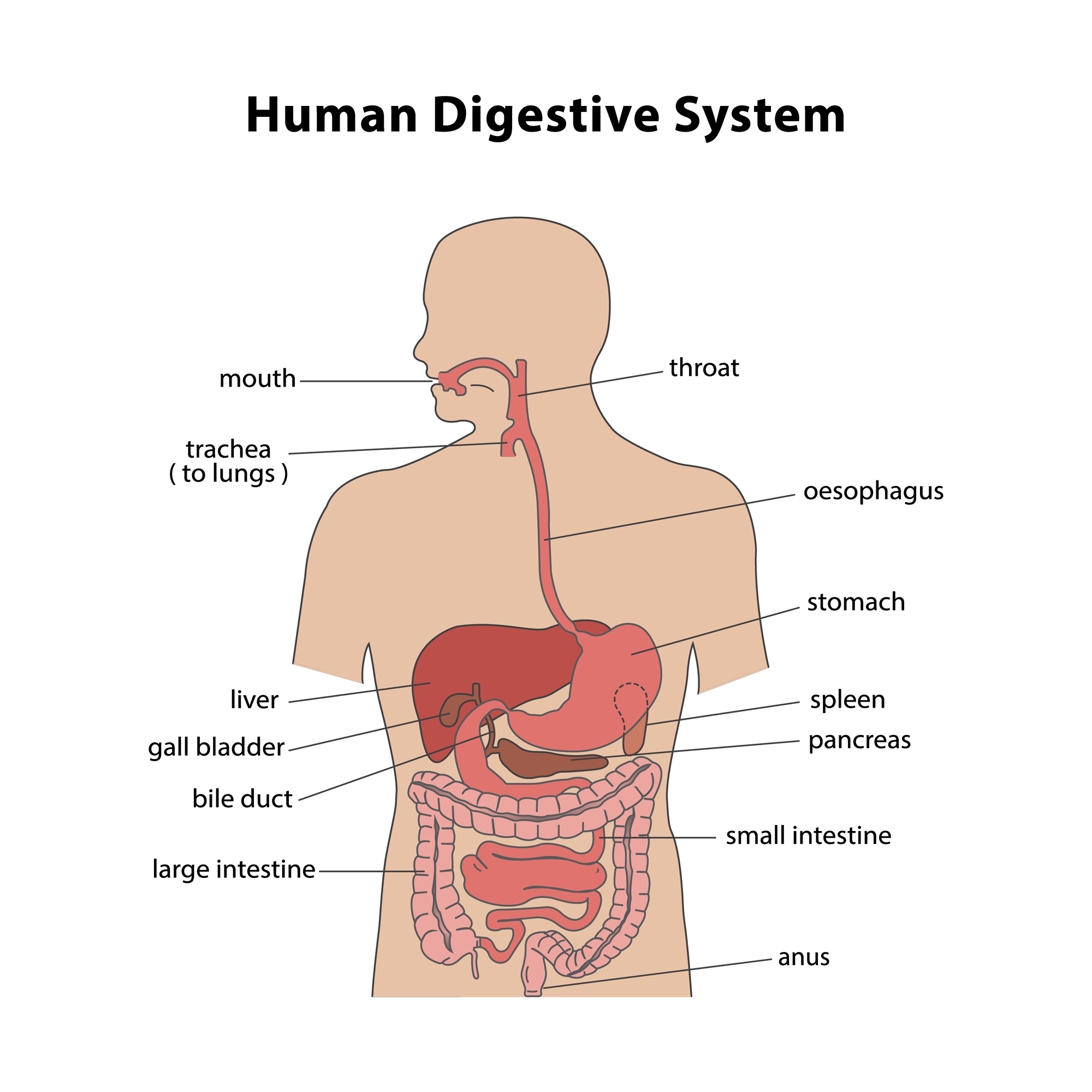
A. Constipation
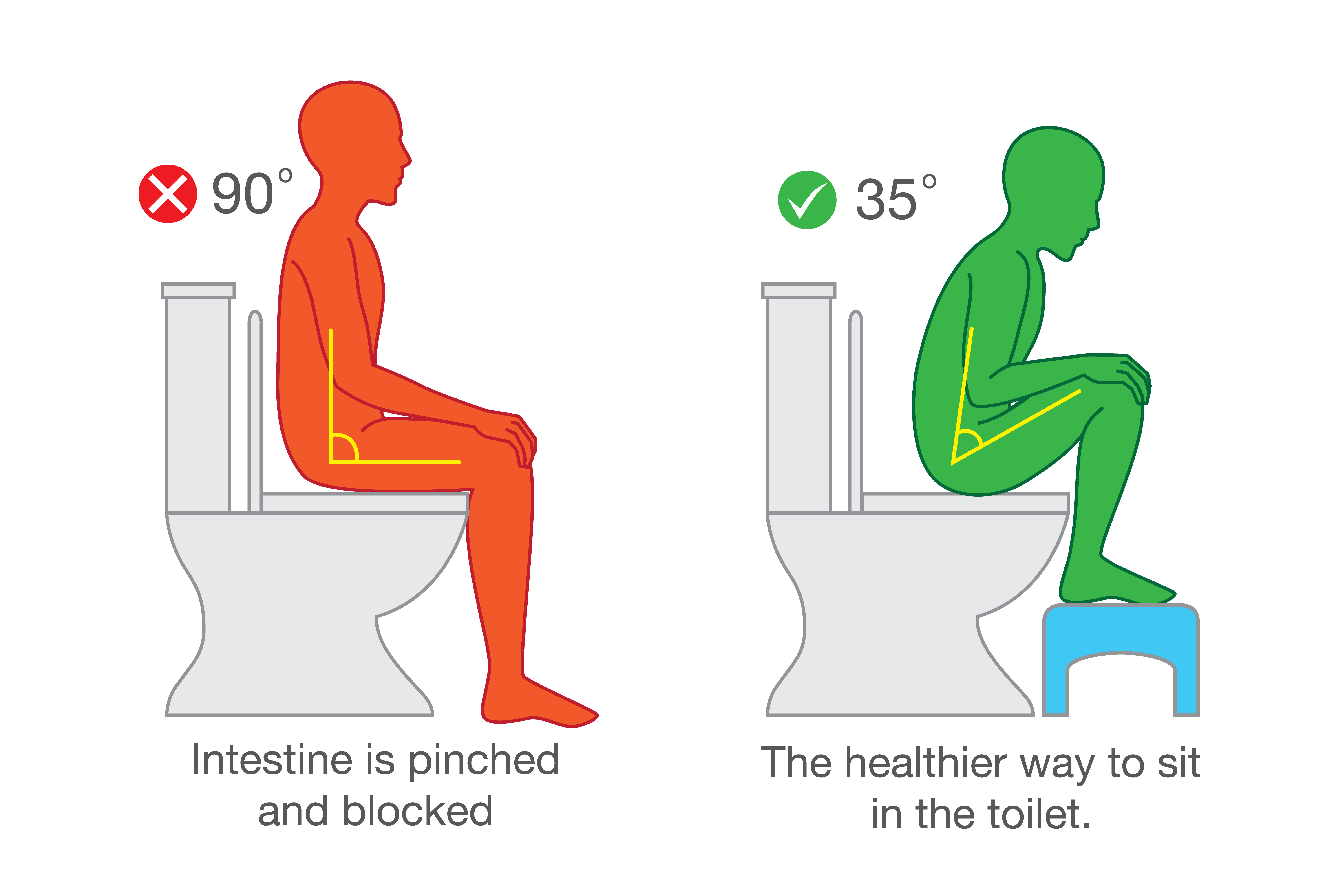
You may be offered a medicine called a laxative. This will help you to poo. More information can be found on the NHS laxative webpage (this link will open in a new tab). You may also be given advice on your:
Toileting routine and correct positioning on the toilet
B. Loose poo (diarrhoea)
C. Farting or wind (flatulence)
They also have a 'poo-torial'. The link opens in a new tab. This gives information about what to look out for in your poo including:
D. Bleeding from the back passage (rectal bleeding)
E. Pain in and around the back passage
F. Pelvic pain
Other things that may help include:

Visit a dietician
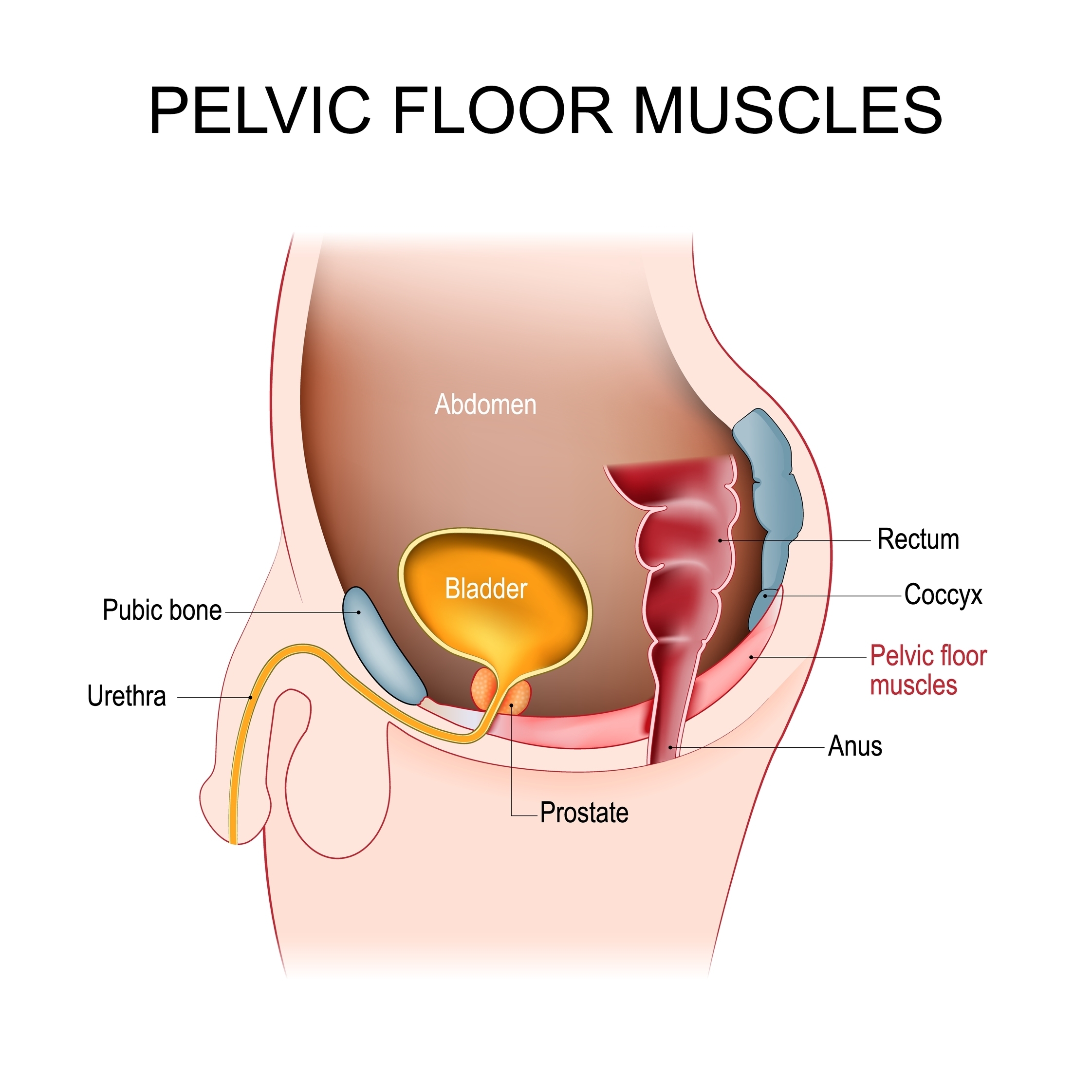
Many issues with peeing, pooing and erections can be helped by strengthening the pelvic floor muscles. The pelvic floor is important in:
In men, the pelvic floor goes from the tailbone (coccyx) to the pubic bone. It supports the bladder and bowel.

Our page on psychological and emotional support gives information on:
There is also a frequently asked questions video in which prostate cancer patient Jamie quizzes consultant clinical psychologist Gail about strategies for coping with the side effects of prostate cancer treatment.
If you can’t pee or find it very difficult to pee.
The toolkit is an information resource for people affected by prostate cancer. The development has been funded through an educational grant from Advanced Accelerator Applications (A Novartis Company).
They have a number of support services that are free to access. For example:
Prostate Cancer UK offer a fact sheet all about the pelvic floor and exercises you can do.
The toolkit is an information resource for people affected by prostate cancer. The development has been funded through an educational grant from Advanced Accelerator Applications (A Novartis Company).