Prostate Biopsy
A prostate biopsy is done to check for prostate cancer.

You would usually have a prostate biopsy if your MRI scan shows an abnormal area.
There are two main types of prostate biopsy.
Transrectal ultrasound (TRUS) guided biopsy. A very fine needle goes through the wall of the back passage (rectum) into the prostate.

Most hospitals are moving towards using transperineal biopsies. This is because there is more chance of infection after a transrectal biopsy. Talk to your doctor about which type of biopsy you are having.

You may be given some antibiotics to take before the biopsy. This will help prevent infection (more common in the transrectal biopsy).
Please let your healthcare team know if you are taking medicines to thin your blood, e.g:
You will need to stop taking these treatments a few days before your biopsies. Please do not stop taking these medications before talking with your healthcare team.

The whole test takes about 20–40 minutes.



Your doctor or nurse should talk to you about any possible risks and side effects before you have the biopsy. If they don’t do this, you can ask them.

Blood in your pee for up to 10 days.

Blood in your semen. This can last for up to six weeks.
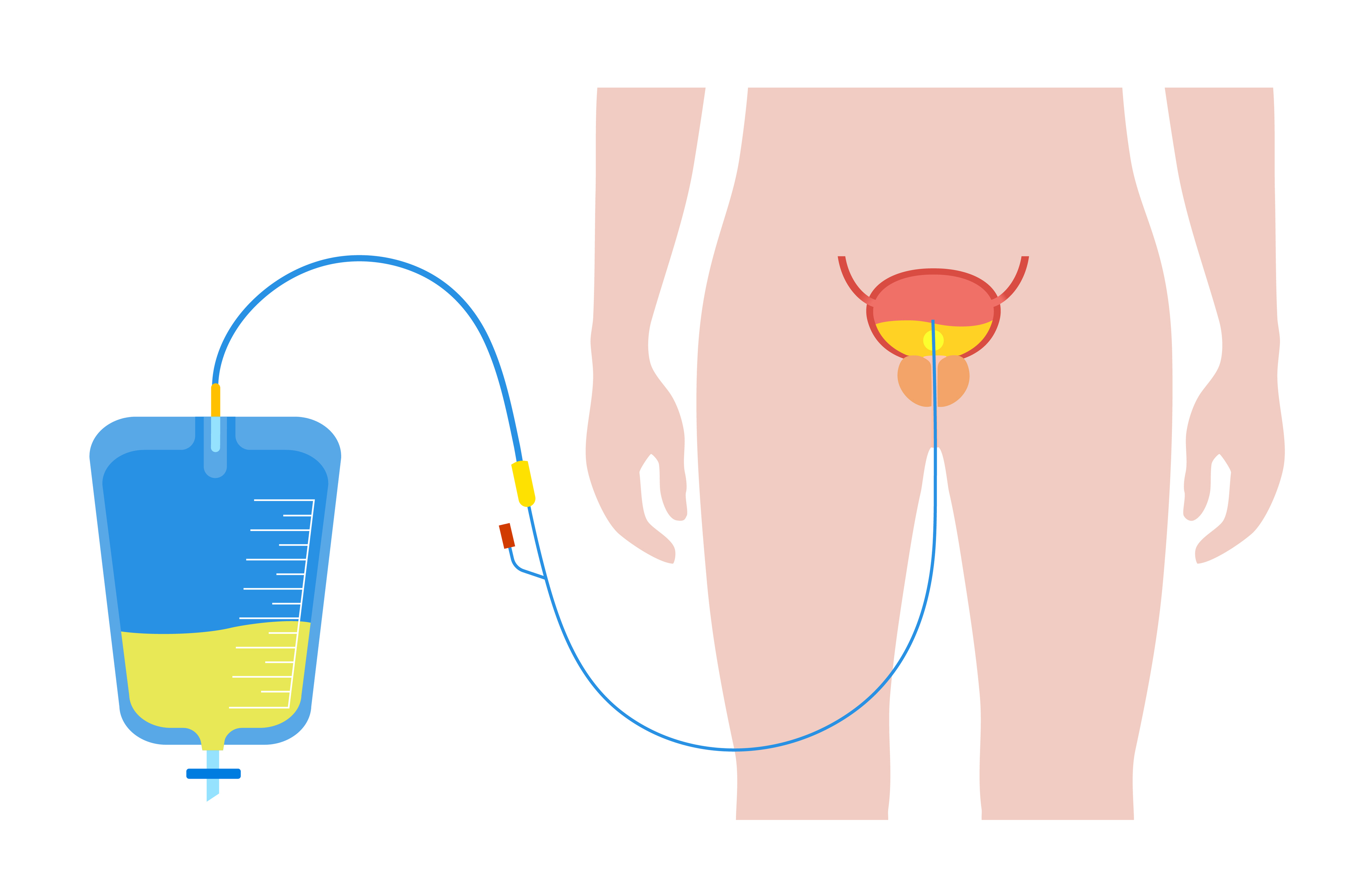
You may be unable to pee. If this happens, please tell your doctor straight away or call 111.
In some cases there is a failure to detect a significant cancer in your prostate.

Blood in your pee for up to 10 days.

Blood in your semen. This can last for up to six weeks.

Blood in your poo.
If your pee is:
or if you have pain when you pass pee, you may have an infection. You will need to speak to your GP.
If you experience any of the following symptoms, you will need to contact your GP or 111 straight away.
Our services search tool (link will open in a new tab) will allow you to search for hospitals near you that offer:
and/or